Synergistic apoptotic effect of celecoxib and lutimax on breast cancer cells
Authors:
Ye-Won Jeon
Young Jin Suh
View Affiliations
Published online on: Thursday, November 29, 2012
Pages:819-825 DOI: 10.3892/or.2012.2158
乳腺癌是异质的,通常是激素依赖性的。有许多乳腺癌治疗选择,包括内分泌治疗,化疗,放射治疗和靶向治疗。不幸的是,并不是所有的患者都对一线治疗有反应,而其他患者最终会复发,尽管有初始反应。这些患者的治疗选择是有限的。在过去十年中,几项研究已经证明塞来昔布和卢特康在乳腺癌中作为单一治疗的抗肿瘤作用。塞来昔布和木犀草素的联合治疗在人乳腺癌细胞中的作用还没有被很好地表征。本研究检查了塞来昔布和卢特康对人乳腺癌细胞系MCF-7和MDA-MB-231的协同效应。我们通过执行细胞存活分析,细胞凋亡分析和蛋白质印迹分析细胞增殖,细胞死亡,凋亡和蛋白质表达的变化。组合治疗显着降低癌细胞活力,并且与以单独的药物或对照以浓度和时间依赖性方式(P = 0.01)的治疗相比,在72小时的治疗后杀死肿瘤细胞具有更大的效率。联合治疗显示大于乳腺癌细胞凋亡的添加性增加(P = 0.01)。在塞来昔布和卢特康组合治疗后观察到Akt磷酸化水平降低(pAkt)。塞来昔布和卢特康的组合提供比单独的塞来昔布或卢特康治疗更好的乳腺癌细胞生长抑制。这些结果表明塞来昔布和卢特康组合可能是乳腺癌的新的可能的治疗选择。

乳腺癌在许多国家是一个严重的关注。尽管公共教育,癌症预防和筛查,增加早期诊断和癌症管理的进展,每年有20万妇女发展乳腺癌和超过40,000女性死于乳腺癌在美国(1,2)。由于乳腺癌通常是激素依赖性癌症,靶向内分泌治疗已导致具有雌激素受体(ER)阳性乳腺癌的妇女的结果的显着改善。然而,并非所有患者对一线内分泌治疗有反应,并且尽管对治疗的初始反应,其他患者将最终复发(3)。这些患者的治疗选择是有限的。此外,具有不是人表皮生长因子受体2(HER2)阳性[(即,三阴性乳腺癌(TNBC)]的激素受体阴性乳腺肿瘤的患者占约15%的乳腺癌患者和这些TNBC患者没有从通常良好耐受的抗HER2药物或靶向内分泌治疗策略中受益(4-6)。虽然通过开发新药物和治疗策略已经取得了相当大的进展,但目前的治疗不能引起临床反应这些患者(7)。
在过去二十年中,已经进行了大量努力来鉴定负责这些患者的信号传导机制,并且正在探索针对癌症信号传导途径的新的治疗靶标。环氧合酶-2(COX-2)在大约70%的原位病例和60%的浸润性乳腺癌中过表达,并且侵袭性乳腺癌中升高的COX-2表达导致肿瘤复发增加和患者存活降低(8,9) 。已经显示COX-2特异性抑制剂通过下调前生存信号通路,蛋白激酶B(PKB)/ Akt(10,11)来促进生长停滞并诱导各种癌症包括乳腺癌中的凋亡。 Western New York暴露和乳腺癌研究结果显示,与最近和成人终生非甾体抗炎药物使用相关的乳腺癌风险显着降低(奇数比0.73,95%置信区间:0.51-1.03)(12)。木犀草素,3',4',5,7-四羟基黄酮是存在于许多类型的植物包括水果,蔬菜和药草中的常见的类黄酮,并且用作抗氧化剂,雌激素调节剂和抗微生物剂(13)。研究已经证明,卢特康的抗癌性质与诱导凋亡相关,其涉及氧化还原调节,DNA损伤,蛋白激酶抑制以消除细胞增殖,抑制转移和血管生成(13,14)。
本研究的目的是检查联合治疗塞来昔布和木犀草素在人乳腺癌细胞中的作用,并随后确定作用机制。
Breast cancer is heterogeneous and often hormone-dependent. There are many breast cancer treatment options, including endocrine therapy, chemotherapy, radiotherapy and targeted therapy. Unfortunately, not all patients respond to first-line treatments, and others will eventually relapse despite an initial response. Therapeutic options for these patients are limited. In the past decade, several studies have demonstrated the antitumor effect of celecoxib and luteolin in breast cancer as single treatment. The effect of combination treatment of celecoxib and luteolin in human breast cancer cells has not been well characterized. The present study examined the synergistic effect of celecoxib and luteolin on the human breast cancer cell lines MCF-7 and MDA-MB-231. We analyzed cell proliferation, cell death, apoptosis and changes in protein expression by performing cell survival assays, apoptosis assays and western blotting. The combination treatment significantly decreased cancer cell viability, and it had a greater efficiency in killing tumor cells after 72 h of treatment, compared to treatment with either agent alone or the control in a concentration- and time-dependent manner (P=0.01). The combination treatment demonstrated a greater than additive increase in breast cancer cell apoptosis (P=0.01). Decreased levels of Akt phosphorylation (pAkt) were noted after celecoxib and luteolin combination treatment. The combination of celecoxib and luteolin provided superior inhibition of breast cancer cell growth than either celecoxib or luteolin treatment alone. These results suggest that celecoxib and luteolin combination may be a new possible treatment option for breast cancer.
Introduction
Breast cancer is a serious concern in many countries. Despite public education, cancer prevention and screening, increase in early diagnosis and advances in cancer management, 200,000 women develop breast cancer and more than 40,000 women die of breast cancer in the United States annually (1,2). Since breast cancer is typically a hormone-dependent cancer, targeted endocrine therapy has led to a significant improvement in the outcomes for women with estrogen receptor (ER)-positive breast cancer. However, not all patients respond to first-line endocrine treatment, and other patients will eventually relapse despite an initial response to the treatment (3). Therapeutic options for these patients are limited. Additionally, patients with hormone receptor-negative breast tumors that are not human epidermal growth factor receptor 2 (HER2)-positive [(i.e., triple-negative breast cancer (TNBC)] account for ~15% of breast cancer patients and these TNBC patients have not benefitted from generally well-tolerated, anti-HER2 drugs or targeted endocrine treatment strategies (4–6). Although considerable progress has been achieved through the development of new drugs and treatment strategies, current therapy is unable to elicit a clinical response in these patients (7).
In the last two decades, there have been major efforts to identify the signaling mechanisms responsible for these patients, and new therapeutic targets are being explored against cancer signaling pathways. Cyclooxygenase-2 (COX-2) is overexpressed in approximately 70% of in situ cases and 60% of invasive breast cancer, and elevated COX-2 expression in invasive breast cancer leads to increased tumor recurrence and decreased patient survival (8,9). COX-2-specific inhibitors have been shown to promote growth arrest and induce apoptosis in various cancers, including breast cancer, by down-regulating the prosurvival signaling pathway, protein kinase B (PKB)/Akt (10,11). The Western New York Exposures and Breast Cancer Study results showed a significant reduction in breast cancer risk associated with recent and adult lifetime non-steroidal anti-inflammatory drug use (odd ratio 0.73, 95% confidence interval: 0.51–1.03) (12). Luteolin, 3′, 4′, 5, 7-tetrahydroxyflavone, is a common flavonoid that exists in many types of plants including fruits, vegetables, and medicinal herbs and acts as antioxidants, estrogenic regulators, and antimicrobial agents (13). Studies have been demonstrated that the anticancer property of luteolin is associated with inducing apoptosis, which involves redox regulation, DNA damage, protein kinase inhibition to cancel cell proliferation, and suppression of metastasis and angiogenesis (13,14).
The objective of this study was to examine the effect of combination treatment of celecoxib and luteolin in human breast cancer cells and to subsequently determine the mechanism of action.
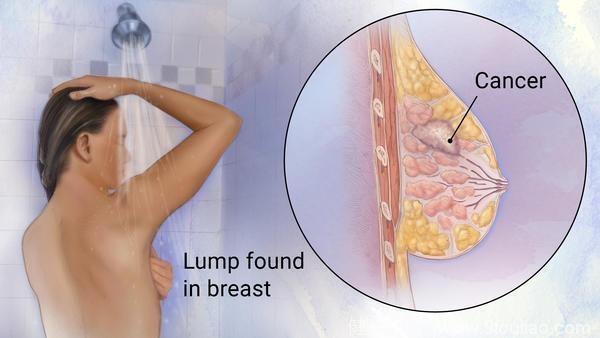
乳腺癌是女性最常见的恶性肿瘤之一,据资料统计,发病率占全身各种恶性肿瘤的7-10%。它的发病常与遗传有关,以及40—60岁间、绝经期前后的妇女发病率较高。通常发生在乳房腺上皮组织。女性居多,男性乳癌占全部乳癌患者的0.5%到1%。
乳腺癌是女性最常见的恶性肿瘤之一,据资料统计,发病率占全身各种恶性肿瘤的7-10%。它的发病常与遗传有关,以及40—60岁间、绝经期前后的妇女发病率较高。通常发生在乳房腺上皮组织。女性居多,男性乳癌占全部乳癌患者的0.5%到1%。
全球每一年有135万新增加的乳腺癌,其中有42万死亡,每年递增是2%。在西欧、北美等发达国家,乳腺癌发病率居女性癌瘤的首位。美国是乳腺癌全球最高发的国家,乳腺癌已经是女性肿瘤的首位,是肿瘤死亡的第二位。一位女性终生患乳癌的危险性是七分之一,每七个人里有一个女性会患乳腺癌。而且这种发病的风险是随着年龄的增加而上升的。中国,本来是低发国,但是最近20年,每年的递增速度是4.6%。中国大、中城市(特别是沿海城市)比农村及内陆地区发病率高,在北京、上海等大城市已经是女性肿瘤的首位,在农村目前是第五位。据统计,中国每年有4万多妇女死于本病,乳腺癌已成为严重威胁女性生命的严重疾病之一。
近年的临床治疗发现:乳腺癌的十年存活率平均达百分之六十,第一期乳腺癌治疗后的存活率达百分之八十,零期乳腺癌治疗后的存活率更接近百分之百,因此早期发现及治疗非常重要。
全球每一年有135万新增加的乳腺癌,其中有42万死亡,每年递增是2%。在西欧、北美等发达国家,乳腺癌发病率居女性癌瘤的首位。美国是乳腺癌全球最高发的国家,乳腺癌已经是女性肿瘤的首位,是肿瘤死亡的第二位。一位女性终生患乳癌的危险性是七分之一,每七个人里有一个女性会患乳腺癌。而且这种发病的风险是随着年龄的增加而上升的。中国,本来是低发国,但是最近20年,每年的递增速度是4.6%。中国大、中城市(特别是沿海城市)比农村及内陆地区发病率高,在北京、上海等大城市已经是女性肿瘤的首位,在农村目前是第五位。据统计,中国每年有4万多妇女死于本病,乳腺癌已成为严重威胁女性生命的严重疾病之一。
近年的临床治疗发现:乳腺癌的十年存活率平均达百分之六十,第一期乳腺癌治疗后的存活率达百分之八十,零期乳腺癌治疗后的存活率更接近百分之百,因此早期发现及治疗非常重要。
近年来我国乳腺癌发病率增速居世界第一,10个女性中就有一个患上乳腺癌。
在医生们看来,这跟生活习惯的变化有很大的关系:高糖高脂肪的饮食、熬夜、快节奏的生活、晚婚晚育等等。
“在医学院学习的时候,老师跟我们讲‘女人,该干嘛干嘛’,话糙理不糙。”杜向慧说,从优生优育的角度,医生就都建议女性在年轻时生孩子,这对自身也是一种保护。
怀孕、分娩、哺乳,虽然很辛苦,但这个过程中,孕激素会保护女人,大大增强女人的抗病能力,这种能力越早获得,对于预防乳腺癌越有帮助。
在中国,45~55岁,65岁以上,这两个年龄段是乳腺癌的高发年龄。近年来,省肿瘤医院,30岁以下患者越来越多,乳腺癌发病年轻化的趋势,全国都一样,城市比农村更明显。











